By Grace Vitaglione
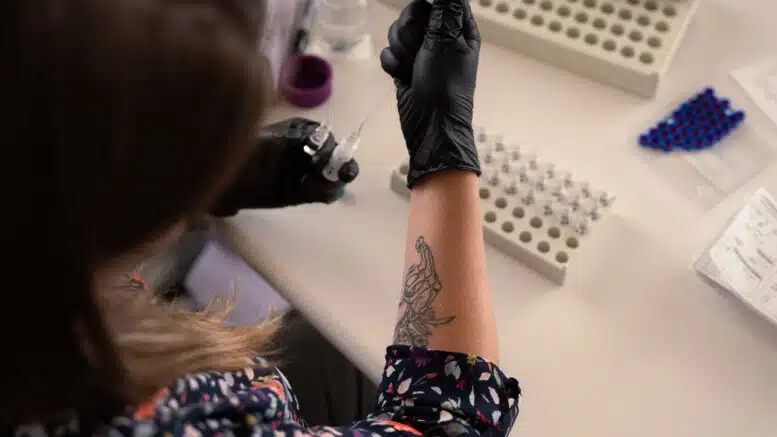
Louise Vincent experienced xylazine, a veterinary tranquilizer, a couple years ago. The drug, commonly called “tranq,” caused wounds on her arms that haven’t fully recovered, she said, and she was ashamed of their appearance.
“It was the most horrible thing I ever experienced,” she said of the painful wounds. At first, she was too embarrassed to seek treatment.
But Vincent, who was raised in Greensboro, has long fought against stigma around substance use. She’s executive director of the North Carolina Survivors Union, a community-led harm reduction organization.
Vincent said she wanted to set an example by not being ashamed. So she stopped hiding the wounds and received treatment, an experience she wrote about for a publication that focuses on substance use issues.
Xylazine can be “devastating,” she said.
And there’s a lot of it in North Carolina’s drug supply.
Now lawmakers would like to regulate the substance. House Bill 563, which would make xylazine a controlled substance, also includes a measure to legalize marijuana for medical use.
Xylazine comes to N.C.
It’s not actually proven whether the drug is driving higher overdose death rates, according to Nabarun Dasgupta, a senior scientist at UNC Chapel Hill. The drug is often used in combination with fentanyl to make its effects last longer, he said.
Many people, though, try to avoid the drug, said Jennifer Carroll, assistant professor of anthropology at North Carolina State University. Some don’t like how it feels or experience negative side effects, she said.
Dasgupta and his team at the UNC Chapel Hill Street Drug Analysis Lab have tracked the drug in N.C. since 2021. As of June 11, they found xylazine in almost a quarter of samples, and it had shown up in 22 of 48 North Carolina counties included in Dasgupta’s survey. Xylazine first appeared mostly in the Triad region, then in the eastern part of the state, then in the west, he said.
Vincent’s organization has also seen this uptick. Her Greensboro-based organization checks members’ drug supplies using a mass spectrometer, and she reports that they’ve seen more and more xylazine in the street drug supply.
Rates of xylazine in samples of street drugs obtained from Robeson, Cumberland, Guilford, Forsyth and Randolph counties are consistently high, Dasgupta said. Almost half of samples from Wake County contained xylazine as of May 30.
What is xylazine, and what does it do?
Scientists are still studying xylazine, so there’s a lot they don’t know, Dasgupta said.
The drug was previously thought to not be an opioid, because it’s not active at the brain’s mu opioid receptor, which produces the euphoria effect present in other opioids, Dasgupta said. Instead, xylazine is active at the kappa opioid receptors, which are more associated with withdrawal and unpleasant sensations. That makes it an opioid, just not one that produces euphoria, he said.
The U.S. Centers for Disease Control and Prevention’s website lists xylazine as a non-opioid, but Dasgupta said that the agency and others are updating their information.
Withdrawals associated with xylazine typically last one to two weeks longer than other opioids, he said.
Dasgupta and his team are studying why xylazine causes skin wounds — even beyond the site of injection. The injuries can start where the skin is broken, like a scrape or a bug bite.
And someone who smokes the drug rather than injecting it can still develop wounds, he said.
His working hypothesis is that because kappa receptors are heavily distributed in the skin, that’s somehow causing the wounds, he said.
According to the Street Drug Analysis Lab, xylazine wounds can look like blisters, scabs, ulcers and/or dark pieces of dead tissue. The injuries often look worse than they are, Dasgupta said. Still, they heal slowly and must be treated like chemical burns, which means keeping the wounds wet and covered and changing the dressings every two to three days initially.
Because the wounds look so scary, people who come in for substance use disorder treatment with the wounds may be turned away. Treatment centers will say they don’t have the medical staff necessary to manage such a complex wound, Dasgupta said.
But people with no medical experience can be trained on how to take care of the wounds, he added.
If someone is experiencing an overdose from xylazine and fentanyl, Dasgupta said naloxone (brand name: Narcan) will still work. However, when xylazine is involved, the person may not revive right away as when they have only used the more commonly seen opioids. They may remain sedated for about 45 minutes, he said.
That’s why it’s important to count their breaths instead of watching for them to wake up, Dasgupta said.
Does xylazine cause more overdose deaths?
State Sen. Danny Britt Jr. (R-Lumberton) told reporters after a meeting of the Senate Judiciary Committee on June 4 that in many areas, people are starting to use xylazine more than fentanyl. His home county, Robeson, is one of the places where Dasgupta’s group found high levels of the substance in the street drug supply.
“It’s having as many overdoses, if not more, than what fentanyl is,” Britt said.
Dasgupta said his team has found, however, that a combination of xylazine and fentanyl often means the person is exposed to less fentanyl — so the overdose is often less severe when xylazine is involved.
“We do see [fatal] overdose rates going down. And if xylazine were to suddenly disappear from the drug supply overnight, would those rates go back up?” he asked. “The science would say ‘yes.’”
So far, xylazine hasn’t been noted as a “significant cause or contributor to overdose deaths” in North Carolina, according to a state Department of Health and Human Services spokesperson.
Medical examiners test for xylazine when indicated and have identified the drug in some overdose death cases over the past decade, the spokesperson wrote, noting that “it appears almost exclusively in combination with a lethal amount of an opioid, usually fentanyl.”
DHHS also pointed to a 2019 CDC article that found fewer than 2 percent of overdose deaths from 38 states, including N.C., were positive for xylazine.
“If you really look at the scientific literature and you’re on top of what’s being published right now, the conclusion would be that this is not what’s driving the overdose death rate,” Dasgupta said.