By Rachel Crumpler
A 31-year-old Asian American woman hopped into an Uber on a mission — to head to a pharmacy in New Bern to get birth control.
Because of her family’s cultural and religious beliefs, she was not allowed to go to doctors’ appointments alone nor to ask for contraception.
But pharmacists’ new ability to prescribe hormonal contraception in North Carolina gave her the opportunity to get connected to the pregnancy prevention method for the first time.
Anna Baird, the pharmacist working that day at Realo Drugs, a community pharmacy with 18 locations in Eastern North Carolina, helped counsel the patient through her birth control options and educated her on sexually transmitted diseases and condoms — topics she hadn’t been able to openly discuss with her family or medical providers.
The patient walked out of the pharmacy with contraception. For Baird, who recently told that story during an interview with NC Health News, it was an invaluable opportunity to reach a patient.
“She is my ‘why,’” Baird said, when also recounting the story to other pharmacists. “We need to be able to provide care to those that are unsupported.”
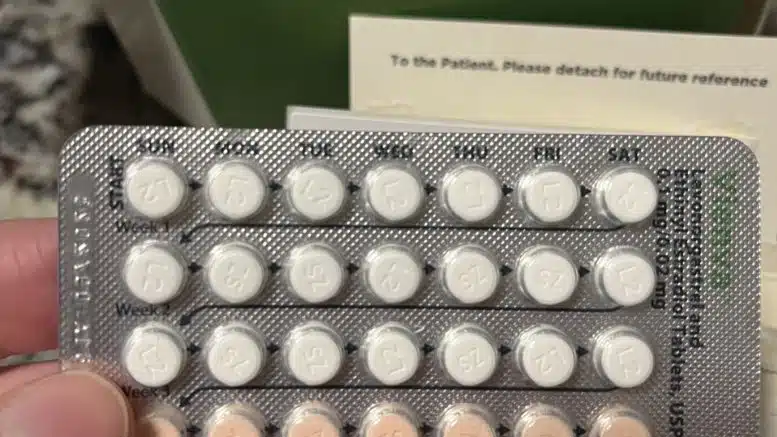
Under a new law, House Bill 96, that went into effect Feb. 1, 2022, pharmacists in North Carolina gained the ability to provide hormonal contraceptives — the pill or patch — to people 18 years and older, as well as those younger with parent or legal guardian consent.
Baird is among the first pharmacists in the state to start providing this service.
“If I think about reproductive health access as a pie, we’re just one new slice of that pie,” said Mollie Scott, UNC Eshelman School of Pharmacy regional associate dean, who is leading a project that supports the implementation of pharmacist-provided hormonal contraception across the state. She said there are different ways for people to access care — from family physicians, obstetrician/gynecologists, county health departments and more. “We’re one additional door that we want to open.”
Twenty-eight states and the District of Columbia allow pharmacists to provide contraceptive care, according to Guttmacher Institute, though the language of the laws governing the practice varies from state to state.
Scott said that, as of March, 564 North Carolina pharmacists completed the required training and are confirmed as providers with the state’s Board of Pharmacy. About 47 pharmacies provide the service, she said.
Over the next few years, Scott expects that number to grow as pharmacists step into new territory to provide hormonal contraception at a time of significant change in reproductive health care access post-Roe.
To that end, on Aug. 11, dozens of stakeholders — pharmacists, state health department staff, physicians and more — gathered for a contraception summit in Chapel Hill to discuss how to improve pharmacists’ participation in providing hormonal contraception across the state.
Combating contraceptive deserts
Amid increased restrictions on abortion, getting contraception has become a more important topic for many women.
“With our evolving landscape around reproductive health, it’s more important than ever that we’re sure that people have that control over their reproductive health and … have access to that full scope of reproductive life planning,” State Health Director Betsey Tilson said at the summit.
In 2020, over a quarter of U.S. pregnancies were unintended, according to America’s Health Rankings. Among unintended pregnancies, 95 percent occur in women who do not use contraception or use it inconsistently or incorrectly.
In North Carolina, 637,960 women with low income live in areas that can be classified as “contraceptive deserts,” according to data from the nationwide pregnancy prevention advocacy group Power to Decide. A contraceptive desert is a county or area that lacks reasonable access to a health center that offers the full range of contraceptive methods.

Furthermore, Tilson, one of the top health officials in the state, said accessing the health care system can be difficult — even for those with resources.
“Even me, trying to access the health care system for my daughter for contraceptive care — we had barrier after barrier,” Tilson said.
Now, pharmacies can serve as an additional access point where hormonal contraceptives can be obtained. Scott said this puts pharmacists in a position to help combat access issues and contraception deserts at a critical time.

“One of the things that I really like about this model is that you may or may not have access to a doctor’s appointment today, or you may have to drive far to get to a doctor — especially if you live in small rural communities — but everybody lives close to a pharmacy,” Scott said.
Almost 90 percent of the U.S. population lives within five miles of a community pharmacy, a 2022 study found. Research shows people may opt to get contraception at pharmacies because they are nearby, have extended hours and don’t require appointments.
“Empowering and resourcing pharmacists and pharmacies to be part of that care team, to help decrease those barriers to care, is really incredibly important,” Tilson said, celebrating the policy advancement.
Need a way to pay
North Carolina is still in the early implementation stage of pharmacist-prescribed contraception, working toward the initial goal of having at least one pharmacist providing the service in each of the state’s 100 counties.
While Baird, the pharmacist in New Bern, jumped at the opportunity to receive training and implement this service at Realo Drugs, many pharmacists have been slower to take action.
There are about 12,000 pharmacists in North Carolina, with 4,723 working in a community setting. So far, as of March — about a year after the law took effect — 1,785 pharmacists registered for the training required to prescribe hormonal contraception.
The NC Board of Pharmacy is paying for the five-hour hormonal contraception training for the first 6,000 pharmacists who sign up to encourage uptake of the service.

Scott said the biggest barrier stopping pharmacists from prescribing hormonal contraceptives is the lack of routine reimbursement for services that fall outside of dispensing a drug, such as time spent counseling.
“We need to establish sustainable reimbursement models because right now we have models that pay for the products but not for the services,” Scott said. “That is something that pharmacists have told us is a need to help them create this new service within their community pharmacies.”
Baird said to provide the service at Realo Drugs, pharmacists charge a $40 consultation fee in line with copays for doctor appointments. She would like to see the reimbursement model change so that the $40 fee could be covered by insurance, rather than the consumer. Until then, the $40 fee could deter some people from going to the pharmacy for this service.
Since last July when the service rolled out, Baird said Realo Drugs has provided about two patients per month with hormonal contraception. She said most patients seeking the service have been between the ages of 18 and 22, getting connected to birth control for the first time. Others have sought a pharmacist to continue their current contraception method in a more convenient manner.
Sign up for our Newsletter
“*” indicates required fields
“Really the convenience factor is the biggest thing for the patients,” Baird said. “We get to meet online and then they come in to finish up the appointment with a blood pressure check. They’re normally out the door in less than 30 minutes.”
Baird expects demand for the service to grow as more people become aware that it exists. But she said even helping two people a month demonstrates a gap that pharmacists are addressing.
Results from Oregon, the first state to implement pharmacist-prescribed contraception in 2016
- Research shows that two years after implementation, the policy prevented more than 50 unintended pregnancies, saving the state approximately $1.6 million in public costs, such as for medical care associated with poor maternal and infant outcomes.
- Among Oregon Medicaid enrollees in the first two years of the program, 10 percent of all new oral and transdermal contraceptive prescriptions were written by pharmacists.
- The safety profile observed with pharmacists was equal to clinicians prescribing contraception.

Ashley Leggett, a pharmacist who has been providing the contraception service at McDowell’s Pharmacy in Scotland Neck, said she felt confident implementing the new service using the hormonal contraception toolkit provided by the NC Association of Pharmacists.
Now, she’s set to open her own pharmacy in Martin County in September, bringing the service over there. She expects her pharmacy may be an especially critical access site for her community after the recent closures of the county hospital and women’s health center.
“My presence in the community is probably going to be pushing this initiative a little bit more because their access to health care, and just reproductive health in general, is very limited,” Leggett said at the summit.
Pharmacists still expect other sites will continue to be the main prescribers of birth control, but they are working to equip themselves to fill gaps.
“This is a way for us to increase access and to be part of that larger reproductive health community to help decrease unintended pregnancies and ultimately decrease maternal mortality,” Scott said.
Over-the-counter contraceptive coming in 2024
- On July 13, 2023, the U.S. Food and Drug Administration approved Opill, the first over-the-counter daily oral contraceptive approved for use in the United States.
- Opill is expected to be available without a prescription at drug stores, convenience stores and grocery stores, as well as online, in early 2024.
- Details about cost have not been announced yet.