By Lee Storrow
Across the globe, scientists, doctors, public health practitioners and community-centered groups are continuing their work to combat the transmission of HIV.
And they’re turning the tide against the disease.
Australia has made historic advancements in this area, and the country is on the verge of eliminating HIV, with new diagnoses of HIV among gay and bisexual men in Australia falling by 57 percent over the past decade. In inner-city Sydney, that number has dropped by 88 percent.
“These encouraging findings from inner city Sydney show just how far we have come since the early days of the AIDS pandemic before we had effective testing, treatment or prevention tools,” Sharon Lewin, IAS President, IAS 2023 International Chair and infectious disease expert at the University of Melbourne in Australia, said in a news release.
This year’s International Conference on HIV Science was in Brisbane, Australia, at the end of July. The location is fitting, given that the country is on track to achieve international 95-95-95 targets: 95 percent of all people living with HIV knowing their status, 95 percent of people diagnosed with HIV receiving sustained antiretroviral therapy, and 95 percent of all people receiving that therapy achieving viral suppression by a 2025 benchmark.
Over the four days of the conference, which is hosted by the International AIDS Society, more than 5,000 representatives from more than 100 countries gathered to share lessons learned, scientific breakthroughs and areas for improvement around the collective efforts to mitigate the transmission of HIV and other communicable diseases.
Keeping an eye on “super gonorrhea”
The COVID-19 pandemic changed the landscape of communicable disease response. This played out at this year’s gathering, where the intersection of HIV with other public health diseases and infections was more apparent at this year’s conference than at previous gatherings.
The public health field also has developed greater understanding of the intersecting syndemic of HIV, hepatitis and other STIs.
One of the biggest shifts in the field of sexually transmitted infections in the past couple of years is related to shifts in treatment of gonorrhea.
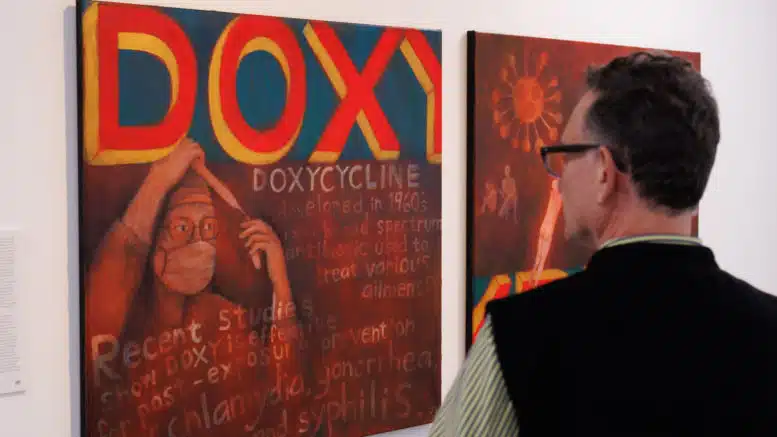
In recent years, a new treatment has emerged to prevent the spread of sexually transmitted infection. The treatment, known as doxyPEP, consists of a dose of doxycycline taken after a sexual interaction and can stop the spread of gonorrhea, along with chlamydia and syphilis.
Scientists at the conference reported that there were still many lingering questions about scaling up the use of doxyPEP. Currently, there is limited information about its effectiveness among women who were assigned female at birth.
There is also significant concern about an increase in antibiotic-resistant gonorrhea if doxyPEP is significantly scaled up. This is not a new concern. In 2012, the U.S. Centers for Disease Control and Prevention announced that it was no longer recommending the oral antibiotic cefixime as treatment for gonorrhea because the pathogen had developed resistance to the antibiotic due to its widespread use.
Eugene McCray, the former director of the division of HIV/AIDS prevention at the CDC, said he was really worried about this “super gonorrhea.”
“I was surprised to learn that ‘super gonorrhea’ has increased so much in recent years and has been spreading rapidly around the world,” said McCray, who graduated from Wake Forest University School of Medicine and completed his medical residency at UNC Chapel Hill.
“Southern states like North Carolina are particularly vulnerable to the spread of this strain due to the large increases in reported cases of Neisseria gonorrhoeae that is occurring, especially among men who have sex with men and persons living with HIV.”
Though there have been no reported cases of drug-resistant gonorrhea in North Carolina, McCray believes it’s only a matter of time before there are reported cases in North Carolina and other Southern states.
“Addressing this threat will require a coordinated clinical and public health response to be sure cases are detected early so we can stop the spread and get people the treatment they need,” said Zack Moore, a physician and the state epidemiologist with the N.C. Division of Public Health. “North Carolina conducts active surveillance for gonorrhea drug resistance via participation in the Strengthening the United States Response to Resistant Gonorrhea project and works with local health departments to ensure access to appropriate testing for drug resistance as needed.”
Science advances while social systems regress
One consistent theme emphasized by North Carolina researchers at the conference was that the biomedical tools at their disposal to confront HIV and other public health diseases have come further than the social systems that influence human behavior.
Chris Beyrer, the director of the Duke Global Health Institute, presented virtually during the conference on human rights protections.
When asked for his key takeaway, he said, “Recent waves of anti-LGBTQ laws, policies and policing in many countries, including Uganda, Tanzania, Ghana, Russia and the United States, are inhibiting the HIV response by driving members of these communities away from health care.
“The advances in HIV prevention and treatment, most importantly with new, long-acting injectable PrEP and antiviral therapy, hold great promise for improving outcomes,” he continued. “But the implementation challenges, importantly including cost and complexity, have led to a stalled, uneven and much too slow rollout of these advances. HIV science has moved far ahead of the health systems needed to make advances usable, equitable and meaningful for those who need them most.”
HIV prevention among young men
On Monday, UNC researcher Nicole Kelly presented her research poster examining the use of pre-exposure prophylaxis (known as PrEP) among young men who have sex with men and the reasons they struggled to take daily PrEP.
Some scientists have assumed this lapse was due to the young men’s developing decision-making skills, but with limited science backing this claim, Kelly, who is an epidemiology PhD candidate at the Gillings School of Global Public Health at UNC Chapel Hill, wanted to test the assumption. The study looked at 225 of young men using daily PrEP, with two study sites in North Carolina, among other locations.
The study showed that messaging that focused on the “risk” of acquiring HIV was not a main driver in young men’s decisions to take PrEP. Instead, Kelly said, “the most common reasons participants listed were actually related to empowerment — youth wanted to be in control of their health and feel safe and healthy.”
To increase use of PrEP among youth, Kelly said it’s important to understand what’s truly driving their decision-making.

“The takeaway is that the message should be about empowerment,” she said. “Trust youth!”
Lee Storrow is the senior director of external affairs at Community Education Group. Before coming to CEG, he was executive director of NC AIDS Action Network for seven years.