By Taylor Knopf
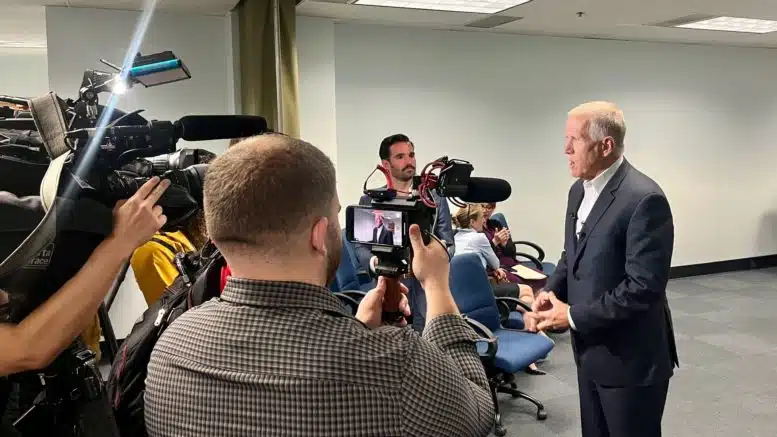
North Carolina’s U.S. Sen. Thom Tillis convened a small group of state health care leaders last week in Raleigh to discuss his legislative agenda about mental health and substance use.
Tillis hosted the meeting during the week of the one-year anniversary of the passage of the Bipartisan Safer Communities Act, the first significant piece of gun violence prevention legislation to make it through Congress in the past 30 years. Tillis was one of the leading Republicans who negotiated the bill in the wake of two mass shootings in Buffalo, New York, and Uvalde, Texas, in May 2022.
In addition to some gun control efforts, the Bipartisan Safer Communities Act authorized billions of dollars in new spending to expand and improve access to mental health services in communities and schools. Last week, Tillis said he didn’t know of any state fully taking advantage of all the new funding streams — and he wants North Carolina to be the first to do so.
“I’m semi-obsessed with making sure North Carolina becomes the nation’s best practice on the implementation of all the behavioral health provisions in BSCA,” Tillis said.
He asked the two state lawmakers present if the General Assembly could create a study committee to analyze the funding streams.
“We are at our best when we are fully informed,” Tillis said.
Sen. Jim Burgin (R-Angier) explained the difficulty that state lawmakers and legislative staff have faced in trying to sort through all the streams of federal funding and their different requirements. He suggested Tillis make calls to the Speaker of the House of Representatives Tim Moore (R-Kings Mountain) and to Senate Leader Phil Berger (R-Eden) to get a study committee launched.
North Carolina Department of Health and Human Services Secretary Kody Kinsley suggested efforts to align some of the federal funding reporting requirements.
“Every SAMHSA dollar, every CDC dollar, every CMS dollar has a whole different reporting schema . . . has a whole different set of requirements, and for our friends that get money, there is no worse gift than money,” Kinsley said with a laugh, referring to multiple federal agencies, including the Substance Abuse and Mental Health Services Administration, the Centers for Disease Control and Prevention and the Centers for Medicare and Medicaid Services. He explained the lengthy contracting process and regular reporting processes that take place every time funds are doled out.
Kinsley said one piece of the Bipartisan Safer Communities Act that North Carolina has really taken advantage of is the expansion of certified community behavioral health clinics. As a result of attempts to restructure the mental health system decades ago, community-based mental health care waned, leading many patients to over-rely on emergency and crisis services. For years, advocates and health leaders have called for more community-based care rather than pushing people into hospitals and long-term facilities to receive mental health services.
Permanent telehealth policies
“I’d like to talk about things that help me focus on the next activities that we should be doing in Washington,” Tillis said.
He said his sights are set on making the telehealth allowances made during the pandemic permanent. Those allowances have been incrementally extended through the pandemic, creating a lot of uncertainty for providers.
“A two-year extension means you’re fundamentally going to use the same technology used today,” Tillis said. “You’re not going to invest in brick and mortar, you’re not going to expand access.”
Tillis said he believes telemedicine was “stress tested” during the pandemic at a large scale, and the bad things people feared might happen with remote medicine didn’t happen. He said he wants to go back to Washington and lay the groundwork for not only authorizing current practices but also paving the way for innovation and expansion of services.
President Joe Biden’s administration recently announced a $40 billion grant program to enhance broadband country-wide that will likely help make more telemedicine possible.
“It’s something where I think the efficacy has been proven. We need to make that standard operating procedure,” Tillis said, before turning the conversation to the group and asking what the next generation of telehealth would look like.
Robyn Jordan, a UNC psychiatrist who also represented North Carolina Medical Society at the meeting, said telehealth has changed how she and her team deliver addiction medicine.
“We take people from all over the state now, whereas we couldn’t do that before,” she said. And she can see them in their home environment, which gives insight into how they are living and if they are keeping up basic hygiene. She’s also able to see people who are homeless or do not have transportation.
“If that were reversed, I believe it would be devastating to the addiction space, because so many people would lose care without telehealth,” she said.
Stephen Lawler of the North Carolina Healthcare Association said telehealth is considered “best practice” in many cases now and is a huge benefit to rural communities that can now connect with health providers in other parts of the state.
When talking about health care innovations, Lawler also brought up insurance providers.
“I think we have to have adequate networks and adequate payment to ensure that no one is being left behind because there’s a barrier to access because somebody is out of network,” he said.
Mental health providers have long said they need to have adequate insurance rate reimbursements to provide and expand their services. There has been a lot of gray area when it comes to insurance reimbursement of telehealth services. Meanwhile, there have been federal parity laws in place for a long time that require payers to cover mental health and substance use services at the same level as other health services. Often that doesn’t happen, and the parity laws go unenforced.
Tillis said he believes there should be parity when providing telehealth services — the same as any other doctor’s visit. Insurance coverage of telemedicine services is something he said would need to be considered moving forward.
Tackling stigma
Another issue Tillis asked to hear feedback about from the group was the ongoing stigma around mental health diagnoses and treatment.
The senator shared a story of a mental health crisis he experienced during his first term as a state lawmaker in the General Assembly. He said he had a health issue that required him to take 90 milligrams of steroids a day for an extended period of time.
“My otherwise quiet demeanor was a little bit ratcheted up. But over the course of six months, I personally experienced pharmacologically induced mania followed by serious depression,” he said. “I don’t think any of my colleagues knew what I was struggling with in the legislature.”
At a later date, Tillis said he wanted to share about his experience at a mental health conference and his staff at the time hesitated, suggesting that maybe he shouldn’t.
“So I know we got a lot of work to do, because I can’t tell you how many times I’ll have somebody come up while doing all this work on mental health and then whisper that they’ve got a family member or friend that’s going through it,” Tillis said. “So what more can we do? Or what more should we do as a matter of policy?”
Ripple Sekhon, a physician with the U.S. Department of Veterans Affairs, said there remains a huge issue around stigma in the military. She often hears about veterans who don’t want a mental health or substance use diagnosis to be recorded in their medical charts for fear of backlash. From there, it’s hard to get them treatment, she said.
Jordan, an addiction medicine psychiatrist, said the stigma around addiction is still stronger than the stigma of mental health, and, at times, the mental health community stigmatizes addiction. She said one policy change that has greatly improved addiction stigma is the removal of a federal waiver that health providers were required to have to prescribe medication for substance use disorders. Since that requirement was lifted, she said more providers have been interested in taking the training to prescribe the medication, and they’re now seeing addiction medicine prescribing just like any other type of prescribing.
Sign up for our Newsletter
“*” indicates required fields
She added that another recent policy change that reduced stigma around addiction was the U.S. Department of Justice’s updated guidance issued last year saying it violates the American with Disabilities Act to discriminate against someone taking medication for opioid use disorder. Jails, health facilities and doctor’s offices cannot refuse someone care or access to medication for substance use disorder.
Jordan said she believes an organization will probably need to be sued in court for this new guidance to fully play out and take effect, but that it’s “a step in the right direction for removing the stigma.”