By Anne Blythe
Amanda Stroud has a passion for public health — an enthusiasm that’s so palpable many of her peers in dentistry describe it as contagious.
As the dental director at AppHealthCare, which serves Ashe, Alleghany and Watauga counties, Stroud is familiar with the challenges of providing oral health care to many in the western part of the state.
Too often, dentists at the federally qualified health center she’s affiliated with wind up having to refer patients who need wisdom tooth extractions, root canals or other complicated oral health procedures to other practitioners.
Many of the patients are economically disadvantaged and have transportation challenges or work schedules that make it difficult to keep such appointments. Sometimes they end up in emergency rooms with dangerous infections because they waited too long to get care.
With that in mind, Stroud began to pose questions to oral health care providers across the state several years ago about how she and her colleagues could avoid having to make so many referrals, which presented yet another access obstacle to health care.
“I started what I call ‘water cooler conversations,’” Stroud said during a recent phone interview.
Those conversations brought a stream of ideas from a number of people that resulted in a “mini residency” pilot program launched in late March by the North Carolina Oral Health Collaborative and the Mountain Area Health Education Center, or MAHEC.
Getting to the nitty gritty
Zachary Brian, a dentist with a dual appointment at the UNC Chapel Hill Adams School of Dentistry and the Gillings School of Global Public Health, was one of the early movers and shakers behind the idea. He was director of the oral health collaborative at the time.
Steve Cline, interim vice president of the collaborative and a dentist with an extensive background in public health, is enthusiastic about the partnership with MAHEC and the potential to expand the prototype statewide.
The goal is to help train “safety-net dentists,” those who care for a population that generally lacks private dental insurance and is unable to pay out of pocket for oral health services.
Stroud and two other western North Carolina dentists from safety net facilities are in the first cohort to receive hands-on clinical training with classroom instruction.
“She was one of the first to say, ‘Can’t we do more?’ ” Cline recalled in a recent phone interview. “We’re trying to get these dentists comfortable with doing these procedures. We’re hoping if this works, we can do more of these in other parts of the state.”
Lack of providers
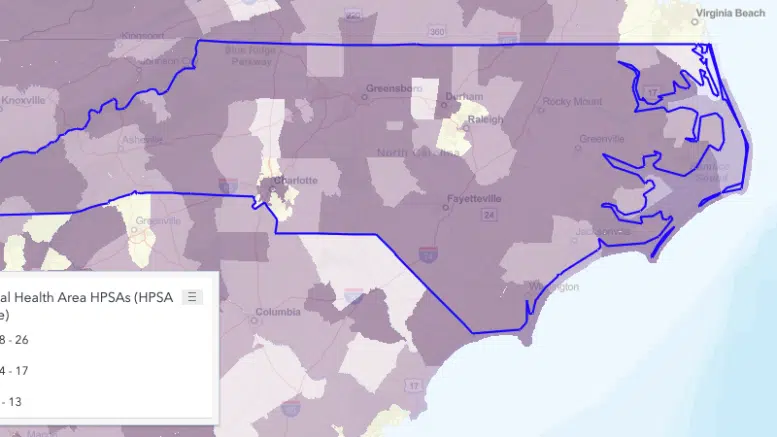
In 2020, data released by the federal Health Resources and Services Administration, showed that 98 of North Carolina’s 100 counties were designated Dental Health Professional Shortage Areas. Counties are given such designations when they don’t have enough oral health professionals to meet the needs of the entire county.
Some of the county features that contribute to such a classification include geographic, transportation and economic challenges, according to the oral health collaborative.
Although Orange and Stokes counties were the only two that did not meet the definition, some counties such as Mecklenburg and Wake were designated shortage areas even when parts of the county had enough dentists to meet needs of a swath of the population.
Further complicating the picture is how few dentists accept Medicaid and underinsured patients. Even if they do, according to public health dentists, it’s often a limited number because of low Medicaid reimbursement formulas.
That puts pressure on health centers such as the one where Stroud and others work to tend to the often more complicated needs of patients whose visits to a dentist are not routine. Some of the children they see have never been to a dentist.
Even though the dentists in the facilities have been through dental school at universities and been taught many of the procedures in school, if they don’t do wisdom tooth extractions, root canals or other complicated procedures regularly in their day-to-day practice, they might lack the confidence to provide such care.
Amadeo Valdez, director of the MAHEC general dentistry residency program, said such procedures can be intensive. The mini residency program is about more than figuring out how to give dentists in his facility the tools to do more.
“You get to know your limitations,” Valdez said, adding that participants get to find that out with the safety net of a more specialized provider by their side.
Stroud, Blaire Mirmow, a dentist at Western North Carolina Community Health Services and Smile America Partners, and Mark Snelson, a dentist at Western North Carolina Community Health Services, showed a willingness to learn during the first weekend of the four-weekend program.
While many dentists take Fridays off, the three were on the MAHEC Biltmore Campus in Asheville.
“These guys were as open as a sponge to get as much as they could.” Valdez said.
A pebble’s ripple effect
The effort to create a continuing education program to help dentists in federal and community health centers was gaining momentum several years ago, then COVID-19 created havoc with many plans.
The creators weren’t idle during the pandemic, though.
“It took a very long time to work through all the legalities,” Katherine Jowers, chair of MAHEC’s Department of Dentistry and Oral Health and associate professor of the University of North Carolina Adams School of Dentistry, said in a phone interview.
Although the pilot project is not a university accredited program, it has been set up and implemented to conform with standards of the American Dental Association Continuing Education Recognition Program.
Sign up for our Newsletter
The mini residency was designed, Jowers said, as one in which the participants could spend much of the week caring for the underserved people in their regions.
“Usually these doctors are actively practicing, and even paying off loans, so going back for a residency isn’t in the cards,” Jowers said in a news release about the program. “Providing them with a ‘mini residency’ in one area of practice, over a few weekends, gives them a longitudinal learning opportunity with both didactic and clinical experiences.”
On April 14 and 15, Jowers said, the selected dentists will practice suturing and tooth extraction on hog jaws.
Even before participating in that class, Stroud said she already is better informed. “I feel more empowered to move forward,” Stroud said.
Stroud lives by the creed to “Do all the good you can, by all the measures you can, in all the ways you can, in all the places that you can, to all the people you can.” The training sessions, she hopes, will allow her and others to do even more good toward evening out the access disparities in quality oral health care.
“It’s like putting a little pebble in the pond and watching the ripple effect,” Stroud said.